Definisi
Tubuh manusia memiliki sistem peredaran darah. Jantung dan pembuluh darah merupakan dua bagian utama yang mendukung sistem tersebut. Pembuluh darah manusia berdasarkan arah aliran darahnya dibagi menjadi pembuluh nadi (arteri) dan pembuluh darah balik (vena). Lebih lanjut, pembuluh nadi akan mengalirkan darah menuju ke seluruh tubuh, tanpa terkecuali pada bagian permukaan tubuh, seperti anggota gerak tubuh (lengan, tangan, paha, betis, dan kaki).
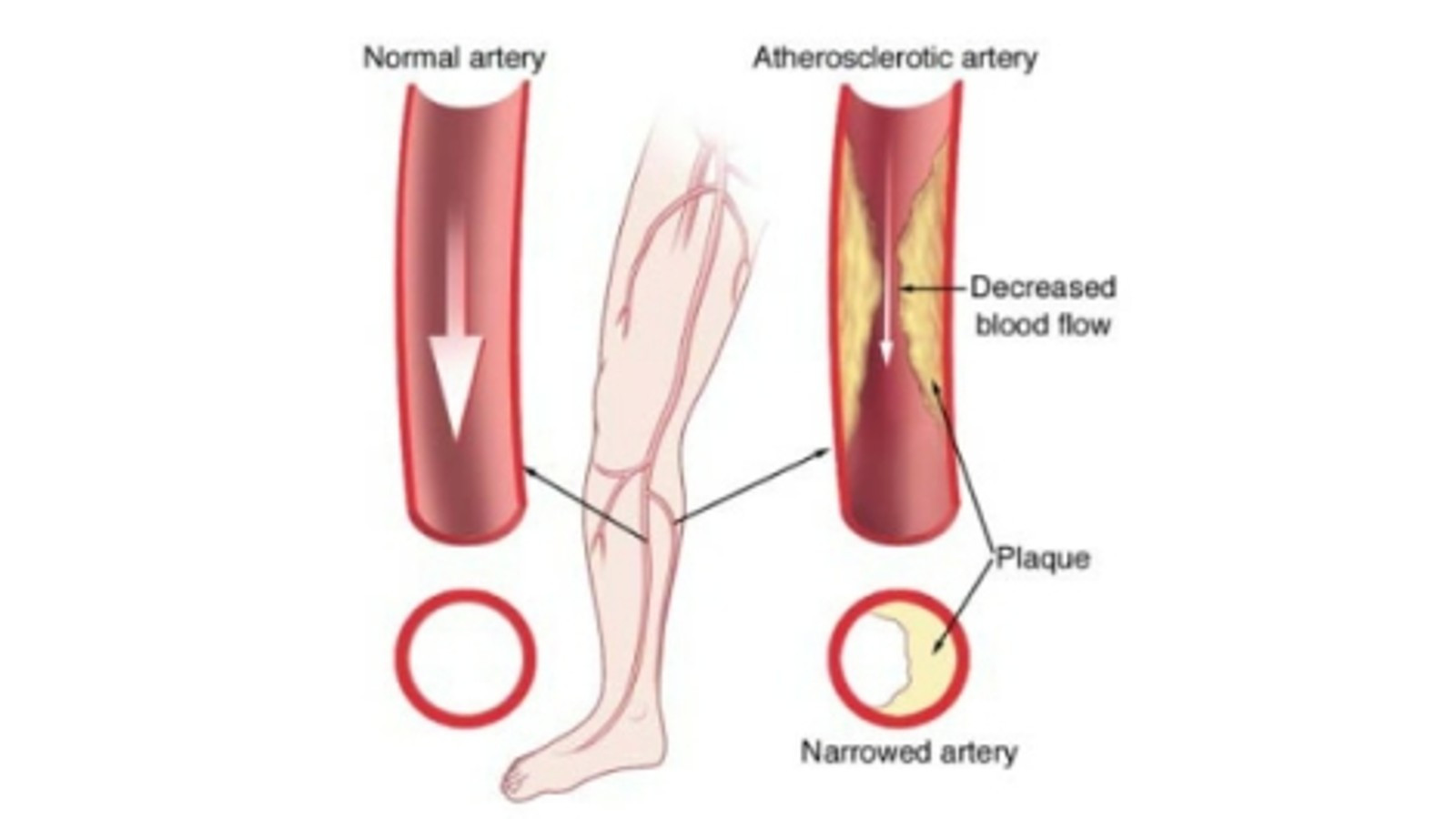
Penyakit Arteri Perifer merupakan kondisi yang terjadi akibat penyempitan pada pembuluh nadi, umumnya pada anggota gerak tubuh, yang mengakibatkan terhambatnya aliran darah ke jaringan tubuh, dalam konteks ini anggota gerak tubuh.
Ketika Anda mengalami gangguan pada pembuluh darah nadi perifer, lengan, tangan, paha, betis, atau kaki Anda akan mengalami kekurangan aliran darah. Padahal bersama aliran darah akan dibawa oksigen dan nutrisi yang akan digunakan sebagai bahan bakar dan sumber makanan dalam pembentukan energi organ-organ tubuh sehingga dapat menjalankan fungsinya dengan baik. Hal ini dapat menimbulkan gejala seperti nyeri pada kaki (klaudikasio) pada saat berjalan.
Penyakit Arteri Perifer juga dapat menjadi pertanda adanya penumpukan lemak pada pembuluh darah arteri atau disebut juga dengan proses atherosclerosis. Kondisi ini dapat menyebabkan terjadinya penyempitan saluran pembuluh darah sehingga mengurangi aliran darah ke jaringan tubuh terutama lengan, tangan, paha, betis, atau kaki. Penyakit ini umumnya dapat diatasi dengan melakukan olahraga rutin, konsumsi makanan bergizi seimbang, dan menghindari kebiasaan buruk seperti merokok.
Penyebab
Penyakit Arteri Perifer umumnya disebabkan oleh proses atherosclerosis. Atherosclerosis disebabkan oleh kerusakan pada dinding pembuluh darah yang mengakibatkan terjadinya penumpukan lemak pada jaringan tersebutn sehingga mengganggu aliran darah karena terjadinya penyempitan pada diameter pembuluh darah.
Penyebab lain yang dapat menyebabkan penyakit arteri perifer berupa peradangan pada pembuluh darah, cedera pada anggota gerak, paparan radiasi dan kelainan pada struktur otot dan jaringan ikat pada persendian.
Faktor Risiko
Beberapa faktor risiko dapat meningkatkan kemungkinan terserang Penyakit Arteri Perifer di antaranya:
- Kebiasaan merokok, kandungan zat nikotin yang ada pada rokok diketahui dapat merusak pembuluh darah dan meningkatkan risiko penumpukan lemak pada lapisan pembuluh darah.
- Obesitas juga menjadi salah satu faktor risiko yang dapat menyebabkan reaksi berantai karena dapat memicu penyakit kronis lain seperti diabetes hingga hipertensi serta tingginya kadar kolesterol dalam darah.
- Diabetes dan hipertensi merupakan penyakit kronis yang dapat menyebabkan rusaknya lapisan pembuluh darah.
- Faktor genetik juga dapat memainkan peran yang penting, terutama pada orang yang memiliki riwayat genetik atau keluarga yang menderita Penyakit Arteri Perifer, penyakit jantung, atau stroke.
- Faktor usia juga dapat menjadi alasan meningkatnya peluang seseorang terkena Penyakit Arteri Perifer. Seseorang diatas usia 50 tahun memiliki risiko lebih mudah untuk mengalami atherosclerosis.
Gejala
Beberapa orang yang menderita Penyakit Arteri Perifer tidak memiliki gejala dan tanda yang signifikan. Namun, penderita penyakit ini cenderung mengalami:
- Sensasi rasa nyeri pada kaki yang dirasakan, terutama pada saat berjalan.
- Nyeri atau kram pada otot kaki maupun tangan yang dipicu oleh aktivitas, seperti berjalan, dan dapat hilang pada saat penderitanya mengistirahatkan kaki atau tangannya. Letak rasa nyeri yang dirasakan bergantung pada lokasi terjadinya penyempitan pembuluh darah. Nyeri pada bagian betis merupakan lokasi yang paling sering dialami oleh penderita penyakit arteri perifer. Tingkat keparahan nyeri yang dirasakan juga dapat beragam. Kondisi ini dapat menyebabkan rasa tidak nyaman hingga rasa nyeri yang mengakibatkan kelemahan anggota gerak. Sensasi nyeri yang parah dapat mengakibatkan Anda kesulitan untuk berjalan atau melakukan beberapa aktivitas fisik.
- Sensasi seperti terasa dingin pada bagian anggota gerak Anda.
- Perbedaan pada warna kulit yang lebih pucat dan mengkilap, terutama jika dibandingkan dua sisi satu sama lain.
- Berkurangnya atau hilangnya pertumbuhan rambut di area yang mengalami Penyakit Arteri Perifer.
- Pada Penyakit Arteri Perifer yang lebih lanjut, rasa nyeri yang Anda rasakan tidak dapat hilang begitu saja meskipun Anda telah mengistirahatkan bagian tubuh Anda yang sakit. Hal ini bisa menjadi masalah yang cukup mengganggu hingga mengakibatkan Anda sulit tidur.
Diagnosis
Dokter akan mengajukan pertanyaan berkaitan dengan kondisi yang Anda alami. Dokter juga akan melakukan beberapa pemeriksaan fisik untuk memastikan penyakit yang Anda derita. Pada pemeriksaan fisik, dokter akan menemukan gejala dan tanda yang spesifik mengarahkan diagnosis kepada dugaan Penyakit Arteri Perifer, seperti melakukan perabaan denyut nadi dan mengukur kekuatan denyut nadi Anda. Dokter juga akan mencari adanya kelainan pada pembuluh darah arteri perifer dengan menggunakan stetoskop. Selain itu, dokter akan mencurigai apabila Anda memiliki luka yang sulit sembuh atau membutuhkan waktu lebih lama untuk sembuh. Kondisi ini dapat merupakan tanda terjadinya penyakit arteri perifer. Lebih lanjut, dokter akan melakukan pemeriksaan tekanan darah pada anggota gerak Anda dan menilai apakah adanya penurunan tekanan pada lokasi yang diperiksa.
Dalam menegakkan diagnosis, dokter membutuhkan pemeriksaan penunjang. Salah satunya yaitu ankle-brachial index (ABI). ABI membandingkan tekanan darah yang ada pada pergelangan kaki dan tangan Anda. Dokter dapat menggunakan alat pengukur tekanan darah biasa atau menggunakan USG untuk menilai tekanan darah dan laju aliran darah. Anda akan diminta untuk berjalan atau menggunakan treadmill dan dilakukan pengukuran sebelum berjalan serta segera setelah selesai berjalan untuk menilai keparahan penyempitan pembuluh darah arteri.
Lebih lanjut, angiografi kateter merupakan prosedur lain yang dapat dilakukan untuk menegakan diagnosis. Prosedur ini dilakukan dengan cara memasukan sebuah kateter melewati pembuluh darah arteri dari paha hingga mencapai lokasi yang dicurigai mengalami penyempitan. Jenis angiografi ini dapat digunakan untuk mengetahui lokasi spesifik terjadinya penyempitan dan mengatasi penyempitan yang terjadi. Setelah menemukan lokasi terjadinya penyempitan aliran pembuluh darah arteri, dokter dapat memasukkan dan mengembangkan balon kecil untuk membantu melebarkan pembuluh darah yang mengalami penyempitan.
Pemeriksaan penunjang lain yang dapat menjadi pilihan adalah pemeriksaan darah. Pemeriksaan ini dilakukan untuk mengetahui adanya peningkatan kadar kolesterol atau trigliserida dan mendeteksi adanya penyakit lain yang dapat mendasari terjadinya penyakit arteri perifer.
Tata Laksana
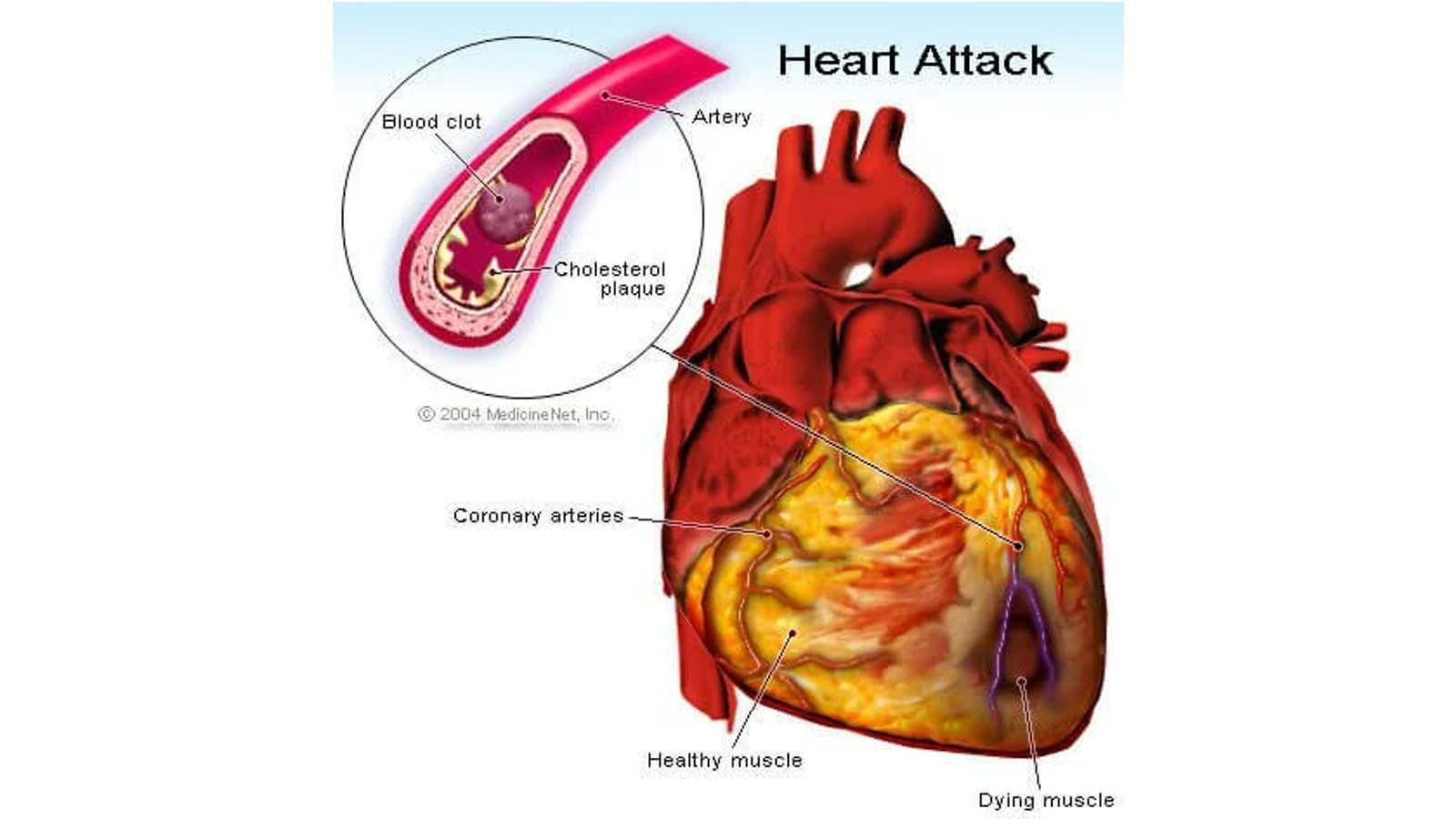
Pengobatan dan terapi yang diberikan untuk mengatasi Penyakit Arteri Perifer memiliki dua tujuan utama, di antaranya adalah untuk mengatasi gejala yang timbul, seperti nyeri sehingga Anda dapat melanjutkan aktivitas sehari-hari tanpa gangguan dan guna menghentikan progresivitas dari penumpukan lemak pada lapisan pembuluh darah yang dapat mengakibatkan penyempitan aliran darah (atherosclerosis). Atherosclerosis dapat meningkatkan risiko terjadinya stroke atau serangan jantung sehingga perlu diatasi agar tidak mengalami komplikasi yang tidak diinginkan.
Dokter akan memberikan obat-obatan untuk membantu menghindari risiko terjadinya penggumpalan darah, menurunkan tekanan darah, menurunkan kadar kolesterol dan mengurangi nyeri serta gejala lainnya yang Anda alami. Apabila Anda mengalami diabetes, dokter juga akan memberikan obat agar kadar gula darah dalam tubuh Anda tetap berada pada ambang nilai normal sehingga Anda terhindar dari risiko kerusakan dinding pembuluh darah.
JIka penyakit arteri perifer disebabkan karena adanya pembekuan darah, dokter akan merekomendasikan pemberian obat yang mengandung zat untuk menghancurkan gumpalan darah yang terbentuk.
Jika dibutuhkan, dokter akan merekomendasikan prosedur pembedahan untuk mengatasi penyakit arteri perifer yang Anda alami. TIndakan pembedahan dilakukan dengan cara membuat jalan pintas pada pembuluh darah yang mengalami penyempitan sehingga aliran darah tidak terganggu. Dokter akan membuat jalan pintas dengan menggunakan pembuluh darah pada bagian tubuh lain yang ditanamkan pada lokasi terjadinya penyempitan.
Komplikasi
Penyakit Arteri Perifer yang tidak ditangani dengan baik bisa menjadi masalah yang serius hingga mengancam nyawa. Beberapa komplikasi diantaranya kematian jaringan yang dapat berujung pada tindakan amputasi, impotensi, rasa nyeri hebat yang mengganggu aktivitas hingga mengakibatkan Anda menjadi sulit tidur, luka yang sulit sembuh dan meningkatkan risiko terjadinya infeksi yang luas atau disebut dengan sepsis. Komplikasi paling serius melibatkan pembuluh darah arteri yang mengangkut darah ke otak dan jantung. Ketika pembuluh darah yang ada di sekitar otak dan jantung mengalami penyumbatan, maka Anda akan mengalami henti jantung, stroke, hingga kematian.
Pencegahan
Tindakan pencegahan yang dapat Anda lakukan dimulai dari perubahan gaya hidup menjadi lebih sehat. Diantaranya adalah dengan berhenti merokok. Rokok merupakan kebiasaan buruk yang dapat memicu terjadinya penyakir arterial perifer hingga memperburuk penyakit yang telah Anda derita dan memperparah komplikasi yang mungkin Anda alami. Selain itu, olahraga teratur juga dapat menjadi solusi untuk mencegah dan meminimalisir risiko terkena Penyakit Arteri Perifer. Konsultasikan dengan dokter untuk menentukan jenis olahraga yang cocok untuk Anda. Selain itu, makan makanan bergizi seimbang juga dapat membantu Anda untuk menghindari risiko tingginya kadar kolesterol atau kadar gula dalam darah Anda.
Kapan Harus ke Dokter?
Segera temui dokter apabila Anda mengalami atau menemukan gejala spesifik yang mengarahkan pada dugaan Penyakit Arteri Perifer. Beberapa gejala yang harus Anda perhatikan diantaranya selain rasa nyeri adalah perubahan warna kulit yang dapat Anda lihat dan amati dengan seksama. Apabila Anda menderita penyakit kronis seperti diabetes dan hipertensi, sebaiknya berkonsultasi dengan dokter dan rajin memeriksakan diri Anda agar dapat mendeteksi sesegera mungkin terkait dengan risiko Anda untuk menderita Penyakit Arteri Perifer.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Anita Larasati Priyono
(American Heart Association, 2021) About Peripheral Artery Disease (PAD) diakses pada 11 April 2022, dari About Peripheral Artery Disease (PAD) | American Heart Association
(CDC, 2021) Peripheral Arterial Disease (PAD) diakses pada 11 April 2022, dari Peripheral Arterial Disease (PAD) | cdc.gov
(Mayoclinic, 2021) Peripheral Artery Disease (PAD) diakses pada 11 April 2022, dari Peripheral artery disease (PAD) - Symptoms and causes - Mayo Clinic
(Mayoclinic, 2021) Peripheral Artery Disease (PAD) diakses pada 11 April 2022, dari Peripheral artery disease (PAD) - Diagnosis and treatment - Mayo Clinic
(Healthline, 2018) Periphjeral Vascular Disease diakses pada 11 April 2022, dari Peripheral Vascular Disease: Types, Causes, and Risk Factors (healthline.com)
(Medscape, 2017) Peripheral Vascular Disease diakses pada 11 April 2022, dari Peripheral Vascular Disease: Background, Pathophysiology, Prognosis (medscape.com)
(NCBI, 2022) Peripheral Arterial Disease diakses pada 11 April 2022, dari Peripheral Arterial Disease - StatPearls - NCBI Bookshelf (nih.gov)
(WebMD, 2021) What is Peripheral Arterial Disease (PAD)? diakses pada 11 April 2022, dari What Is Peripheral Artery Disease (PAD)? (webmd.com)