Definition
Tachycardia is a heart rate that exceeds 100 beats per minute. A rapid heartbeat is not always a cause for concern. For example, the heart rate typically rises during exercise or under stress. Tachycardia, on the other hand, can be classified as one of several types of heart rhythm disorders known as arrhythmia.
Causes
Common causes of tachycardia are:
- Fever
- Excessive alcohol consumption
- Excessive caffeine consumption
- Low or high blood pressure
- Heart damage due to heart attack or heart failure
- Structural abnormalities of the heart such as cardiomyopathy
- Heart valve disease
- Electrolyte imbalances, such as potassium, sodium, calcium, and magnesium
- Side effects of medications
- Hyperthyroidism
- Smoking
- Use of illicit drugs such as stimulants (e.g. cocaine or methamphetamine)
Sometimes the exact cause of tachycardia is unknown. Tachycardias that cause symptoms are classified according to the part of the heart responsible for the increase in heart rate and the cause.
- Ventricular tachycardia. Ventricular tachycardia occurs when abnormal electrical signals from the ventricles cause the heartbeat to accelerate. This can be dangerous as the ventricles play an important role in the body, pumping blood to the lungs and the rest of the body
- Supraventricular tachycardia. Supraventricular tachycardia occurs when abnormal electrical signals come from above the ventricles and cause the heart to beat rapidly.
Risk factor
Tachycardia is more likely in people who are elderly or have a family history of heart rhythm disorders.
Symptoms
A fast heart rate disrupts the blood-filling process in the heart chambers. The ventricles have not yet been filled with enough blood but have contracted to pump it, so the blood channeled throughout the body is insufficient, and the ventricular pump becomes less efficient. As a result, tissues and organs do not receive adequate oxygen and nutrients.
In general, tachycardia can cause the following signs and symptoms:
- A sensation of a racing or pounding heart that comes and goes suddenly
- Chest pain
- Fainting
- Dizziness or feeling of floating
- Rapid pulse
- Shortness of breath
Some people with tachycardia have no symptoms, and it is usually discovered accidentally during a medical examination by a doctor for another reason.
Diagnosis
Tachycardia is typically diagnosed through a physical examination and questions about your medical history and complaints. Several tests may be performed to confirm the presence of abnormal tachycardia and look for potential causes. These tests include:
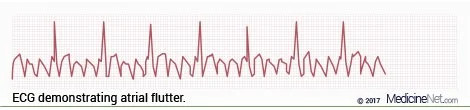
- Electrocardiogram (ECG). This measures the electrical activity of the heart and can reveal the type of tachycardia and heart defects that could be causing it
- Holter monitor. This is a portable ECG for monitoring heart rate at home. It is worn for 24 hours or more to monitor heart rate during daily activities
- Echocardiography. This examination may reveal problems with blood flow, heart valves, and heart muscle
- Chest X-ray. A chest X-ray can show the condition of the heart and lungs
- Cardiac MRI. This examination can produce images of how blood flows through the heart. The images may be still or moving. It is most commonly used to determine the cause of ventricular tachycardia
- CT scan of the heart. It can also be done to determine the cause of ventricular tachycardia
Management
The goal of treatment and therapy for tachycardia is to slow the heart rate and prevent subsequent episodes of tachycardia. If the tachycardia is caused by a specific medical condition, then treating that condition may reduce or prevent tachycardia episodes.
Sometimes, tachycardia goes away on its own, but sometimes it requires other therapies such as:
- Vagal maneuvers. These maneuvers include coughing, straining, and applying ice packs to the face. These can affect the nerves that control the heart rate, causing it to slow down
- Medications. If vagal maneuvers do not help, heart rate control medications may be given
- Electroshock therapy with cardioversion. This procedure involves administering an electrical shock to the heart via a sensor attached to the chest. This shock will affect the electrical signals in the heart and restore them to normal. Cardioversion is usually performed in an emergency or when vagal maneuvers and medications do not work. Cardioversion can also be performed using medication
To prevent further episodes of tachycardia, several treatments can be done:
- Heart rate control medications. These are usually prescribed to most people with tachycardia
- Radiofrequency ablation. This procedure is done to destroy the abnormal heart tissue that causes tachycardia
- Implantable cardioverter-defibrillator (ICD). This device is similar to a pacemaker, but the difference is that an ICD works to restore a heartbeat that is too fast (tachycardia), whereas a pacemaker works to restore a slow heartbeat (bradycardia)
- Surgery
Complications
Complications of tachycardia are determined by:
- What type of tachycardia
- Heart rate
- The length of time the tachycardia lasts
- Presence of other heart diseases
If not treated properly, tachycardia can lead to complications such as:
- Stroke. Tachycardia increases the risk of blood clots forming which can lead to a stroke or heart attack
- Fainting or unconsciousness
- Heart failure due to the heart not being able to pump blood properly
- Cardiac arrest, which can lead to death. These complications are usually only seen with ventricular tachycardia
Prevention
The best way to prevent tachycardia is to maintain a healthy heart and avoid heart disease. If you already have heart disease, keep track of your symptoms and follow your doctor's treatment recommendations. Take the medications prescribed by your doctor on a regular basis.
A healthy lifestyle can reduce the risk of developing heart disease and thus prevent tachycardia. A healthy lifestyle includes:
- Healthy diet. Choose foods high in whole grains, lean meat and skin, low-fat dairy products, fruits, and vegetables. Limit consumption of salt, sugar, alcohol, and saturated fats
- Exercise regularly. Aim to exercise for at least 30 days at least five times per week
- Maintain an ideal body weight. Being overweight and obese increases the risk of heart disease
- Control blood pressure and cholesterol. Adopt a healthy lifestyle and take medications as prescribed by your doctor
- Quit smoking. If you are unable to quit smoking, talk to your doctor about a smoking cessation program
- Drink less alcohol. For healthy adults, the maximum amount of alcohol you can drink is one drink for women and two drinks for men. If you have a medical condition, you may be advised not to drink alcohol at all
- Avoid using illegal drugs or stimulants like cocaine. Contact your nearest healthcare provider if you need help quitting your medication
- Be careful about using medications. Some medications, such as cough and cold medicines, contain stimulants that can cause an increase in heart rate. You should consult your doctor to see if there are any medications that you should avoid
- Limit caffeine consumption. If you do consume caffeine, limit it to no more than four caffeinated drinks a day
- Control stress. Find ways to reduce emotional stress, such as physical activity, meditation, and joining support groups
When to see a doctor?
Some things can cause takikardia. If you feel your heart rate is too fast, you should consult a doctor.
You need to immediately visit health facilities if you experience symptoms such as:
- Shortness of breath
- Dizzy or feeling floating
- Fainted or almost fainted
- Pain or discomfort in the chest
Looking for more information about other diseases? Click here!
- dr Anita Larasati Priyono
Tachycardia - Diagnosis and treatment - Mayo Clinic. Mayoclinic.org. (2022). Retrieved 7 April 2022, from https://www.mayoclinic.org/diseases-conditions/tachycardia/diagnosis-treatment/drc-20355133.
Flutter, thump, bump: facts about tachycardia. WebMD. (2022). Retrieved 7 April 2022, from https://www.webmd.com/heart-disease/atrial-fibrillation/what-are-the-types-of-tachycardia.
Tachycardia: Fast Heart Rate. www.heart.org. (2022). Retrieved 7 April 2022, from https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/tachycardia--fast-heart-rate.