Definition
Sepsis-associated encephalopathy (SAE) is a sudden dysfunction of the brain that occurs in the context of sepsis. Sepsis is the body’s extreme response to an infection, triggering widespread inflammation. It is a medical emergency.
Encephalopathy can occur early in the course of sepsis and is a common neurological complication in septic patients. The presence of encephalopathy in a person with sepsis is a predictor of poor prognosis and increased mortality.
Sepsis and its complications cause more deaths than the combined fatalities from prostate cancer, breast cancer, and HIV/AIDS.
Causes
Sepsis-associated encephalopathy is caused by widespread inflammation in the body during sepsis. This condition arises without direct brain infection or other diseases that can also cause encephalopathy, such as liver and kidney diseases.
In sepsis, widespread inflammation leads to inflammatory substances circulating in the blood, reaching the brain tissues. This causes direct damage to brain tissues through various mechanisms, including metabolic disturbances, oxygen supply impairment to the brain, neural transmission changes, and blood flow disruption to the brain.
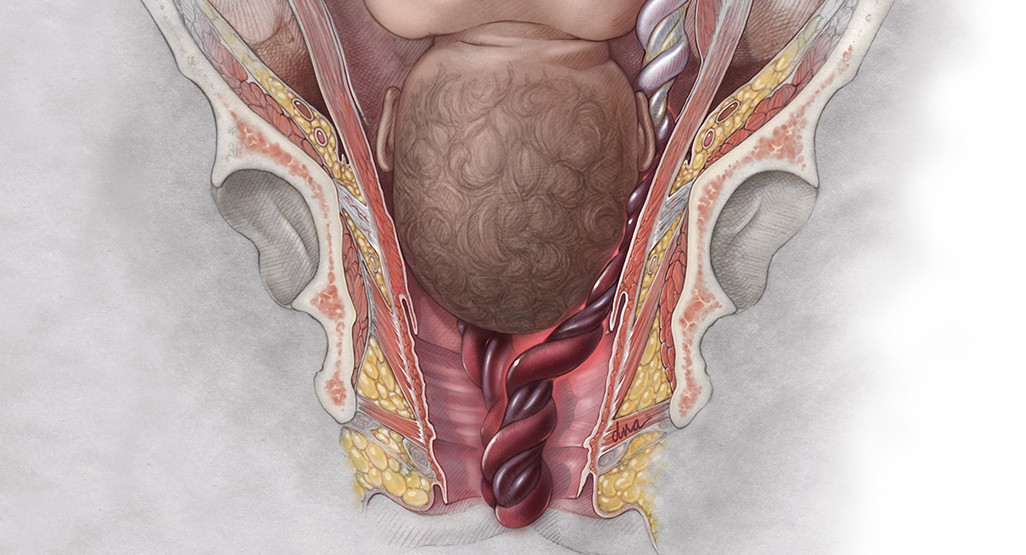
The most common cause of sepsis is bacterial infection, though it can also be caused by fungal, parasitic, or viral infections. The source of infection can originate from any part of the body. Common locations and types of infections leading to sepsis include:
- Abdomen: infections such as appendicitis, intestinal infections, peritonitis, gallbladder infections, or liver infections.
- Lungs: infections like pneumonia.
- Skin: bacteria can enter through wounds or skin inflammation, or via IV lines.
- Urinary tract: urinary tract infections, especially in patients with catheters or urinary tubes.
Risk factor
Sepsis-associated encephalopathy can affect anyone, but some individuals are at higher risk, including:
- Elderly (over 65 years), very young individuals, or pregnant women
- People with certain medical conditions like diabetes, lung disease, cancer, and kidney disease
- Individuals with weakened immune systems such as those with HIV/AIDS, long-term immunosuppressant users (e.g., cancer patients or organ transplant recipients)
- Hospitalized patients
- Individuals with severe injuries, such as extensive burns or other major injuries
- People using IV lines, urinary catheters, or breathing tubes
Symptoms
Symptoms of sepsis-associated encephalopathy include:
- Changes in behavior or personality
- Altered consciousness, ranging from drowsiness to coma
- Restlessness, agitation
- Disorientation
- Depression
- Impaired clear thinking or difficulty focusing thoughts
- Speech disturbances
- Postural abnormalities
- Coordination issues
- Muscle weakness or uncontrolled twitching
- Uncontrolled eye movements
- Tremors
- Swallowing difficulties
- Irregular breathing patterns
- Seizures
Diagnosis
Diagnosis of encephalopathy is made when encephalopathy symptoms are present in someone with an infection other than a brain infection. In addition to symptoms, physical examination findings in sepsis include:
- Fever (temperature usually > 38.3 degrees Celsius)
- Hypothermia (temperature < 36 degrees Celsius)
- Rapid heart rate (> 90 beats per minute)
- Rapid breathing (> 30 breaths per minute)
- Decreased systolic blood pressure (< 90 mmHg) or a drop of > 40 mmHg from the patient’s usual blood pressure
- Reduced urine output per hour
Several tests can help diagnose and rule out other causes of encephalopathy, such as:
- Complete blood count
- Blood culture to detect the bacteria causing sepsis
- Electrolyte tests
- Blood lactate (increased in sepsis), blood ammonia, liver enzymes (to assess liver damage), and bilirubin (increased in sepsis)
- Blood glucose (increased in sepsis)
- Blood oxygen levels (decreased in sepsis)
- Kidney function tests, including blood urea and creatinine
- Coagulation tests
- CT scan and MRI to detect brain swelling, structural abnormalities, or infection
- Electroencephalogram (EEG) to detect brain damage or abnormal brain wave patterns
- Somatosensory-evoked potentials (SSEP)
- Autoantibody analysis, as some dementias are caused by nerve-damaging antibodies (autoantibodies)
However, none of these tests are specific for sepsis, so the diagnosis of sepsis-associated encephalopathy is usually made after excluding other causes of encephalopathy.
Management
Despite its high mortality rate, the treatment of sepsis-associated encephalopathy is limited to addressing the underlying infection and providing therapy for symptom management such as seizures and altered consciousness.
Intravenous antibiotic therapy is the primary treatment and should be initiated immediately after diagnosing sepsis. Early antibiotic administration is associated with lower mortality rates. The choice of antibiotics is controversial and will be based on the patient’s history, such as previous antibiotic use, medical history, and the doctor’s assessment. The doctor will also consider blood culture results showing the specific bacteria causing sepsis.
Before blood culture results are available, doctors will administer broad-spectrum antibiotics such as vancomycin, piperacillin-tazobactam, imipenem-cilastatin, or cefepime. Additionally, other antibiotic classes like fluoroquinolones, aminoglycosides, or monobactams may be added. Once blood culture results are available, these antibiotics may be adjusted to target the specific bacteria. Antibiotic therapy is usually given for at least 7 to 10 days, although it can be longer in patients with slow responses, stubborn infections, or those with weakened immune systems.
Complications
Sepsis-associated encephalopathy can cause persistent cognitive function impairments, affecting the quality of life. The most severe complication of encephalopathy is death.
Prevention
Preventing sepsis-associated encephalopathy involves promptly and appropriately managing sepsis. However, this is not always successful. Therefore, it is better to take steps to prevent sepsis itself, including:
- Practicing good hand hygiene
- Staying up to date with vaccinations
- Regularly consult a doctor if you have chronic (long-term) illnesses
- Seeking immediate medical attention if you suspect an infection
When to see a doctor?
If you or someone else experiences symptoms of encephalopathy, seek medical help immediately by calling emergency services or going to the emergency department. However, do not drive yourself to the emergency department as you may experience a decrease in consciousness.
Looking for more information about other diseases? Click here!
- dr Ayu Munawaroh, MKK
Chaudhry, N. (2014). Sepsis Associated Encephalopathy. Pubmed. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4590973/
Sepsis: Causes, Symptoms, Treatment & Prevention. (2022). Retrieved 22 September 2022, from https://my.clevelandclinic.org/health/diseases/12361-sepsis#prevention
Ren, C., Yao, R., Zhang, H., Feng, Y., & Yao, Y. (2020). Sepsis-associated encephalopathy: a vicious cycle of immunosuppression. Journal Of Neuroinflammation, 17(1). doi: 10.1186/s12974-020-1701-3