Definisi
Cutaneous larva migrans (CLM) atau yang juga disebut dengan creeping eruption adalah penyakit kulit yang disebabkan oleh cacing tambang. Cacing termasuk ke dalam golongan kuman parasit. CLM biasanya ditemukan pada negara beriklim tropis. Penyakit infeksi kulit ini sering terjadi pada orang yang tinggal atau pernah bepergian ke negara tropis.
CLM menempati urutan kedua dari seluruh infeksi cacing di negara berkembang setelah infeksi cacing kremi. Jumlah keseluruhan kasusnya tinggi pada daerah beriklim hangat, dimana orang cenderung berjalan tanpa alas kaki seperti di pantai atau pada komunitas dengan sosio ekonomi yang rendah, serta berkontak dengan kotoran hewan.
Penyebab
CLM disebabkan oleh beberapa jenis larva cacing tambang yang berbeda. Larva adalah bentuk remaja dari cacing tambang. Cacing tambang yang paling sering menyebabkan CLM adalah spesies Ancylostoma. Ancylostoma braziliense yang merupakan cacing tambang pada anjing atau kucing peliharaan, adalah penyebab CLM tersering di Amerika dan Karibia. Selain itu, terdapat juga Ancylostoma caninum atau cacing tambang pada anjing, yang banyak ditemukan di Australia. Parasit hidup dan bertelur di dalam usus hewan peliharaan, seperti kucing dan anjing. Kotoran hewan yang ditinggali akan mengandung telur cacing. Telur kemudian menetas menjadi larva yang dapat menyebabkan infeksi.
Infeksi terjadi ketika larva bersentuhan dengan kulit lalu masuk ke dalam tubuh. Larva banyak dijumpai di tanah atau pasir yang terkontaminasi. Untuk masuk ke dalam tubuh, larva menembus lapisan atas kulit. Orang yang berjalan tanpa alas kaki atau duduk di tanah tanpa penghalang seperti handuk, memiliki risiko yang lebih tinggi untuk terpapar larva cacing tambang.
CLM paling sering dijumpai di daerah beriklim hangat dan lembap seperti Amerika Serikat bagian tenggara, Karibia, Amerika Tengah dan Selatan, Afrika, Timur Tengah, serta Asia Tenggara. CLM juga banyak ditemukan pada tempat dengan sanitasi yang buruk.
Faktor Risiko
Beberapa faktor risiko CLM antara lain:
1. Laki-Laki
Laki-laki tiga kali lebih berisiko mengalami CLM dibandingkan perempuan. Diperkirakan karena laki-laki lebih banyak menghabiskan waktu di luar ruangan, lebih banyak berkontak dengan tanah ketika bermain, dan lebih jarang diawasi oleh orang tua.
2. Usia 10-14 Tahun
Anak antara usia 10-14 tahun memiliki resiko 2 kali lebih besar dibandingkan anak kelompok usia yang lebih kecil. Hal ini disebabkan karena mereka lebih banyak beraktivitas di luar rumah, lebih banyak berkontak dengan tanah ketika bermain, dan sudah tidak diawasi ketat oleh orang tuanya.
3. Terpapar Pasir atau Tanah
Orang-orang yang berjalan tanpa alas kaki lebih mudah terpapar parasit cacing dibandingkan dengan yang memakai alas kaki, meskipun hanya sandal jepit sederhana. Kebiasaan tidak memakai alas kaki ini banyak dilakukan oleh anak-anak terutama saat bermain. Selain itu, pekerjaan yang banyak terpapar pasir atau tanah seperti ekskavasi atau konstruksi.
4. Lingkungan
Banyak faktor lingkungan yang dapat meningkatkan risiko terkena CLM, di antaranya:
-
- Lingkungan luar
- Kotoran hewan yang tidak dibersihkan
- Jalanan yang tidak diaspal
- Banyak hewan liar yang bermain dan buang air di jalan tanpa pengawasan
- Kemiskinan atau pendapatan yang rendah
- Hewan peliharaan belum diberikan obat cacing dan terkontaminasi tanah yang terinfeksi cacing
Gejala
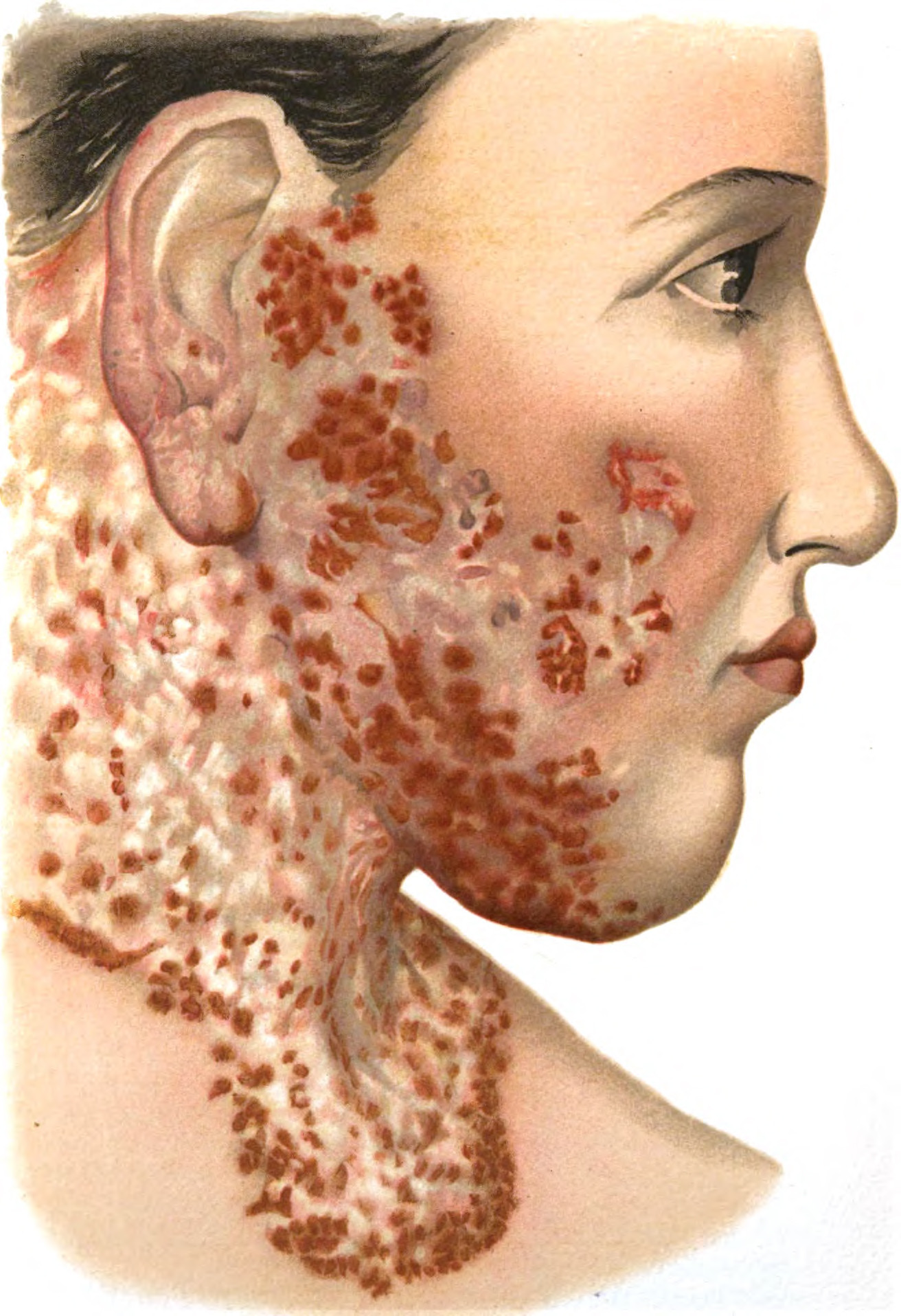
Tanda-tanda CLM biasanya muncul pada hari pertama hingga kelima setelah infeksi, meski terkadang juga butuh waktu lebih lama. Tanda dan gejala yang umum meliputi:
- Lesi atau tampilan tidak normal pada kulit berupa kemerahan dan berkelok-kelok yang terlihat pada kulit. CLM muncul sebagai lesi merah yang memiliki pola seperti ular. Hal ini disebabkan oleh pergerakan larva di bawah kulit. Lesi bisa bergerak hingga 2 cm dalam sehari
- Rasa tidak nyaman, lesi CLM bisa terasa gatal, menyengat, atau menyakitkan
- Pembengkakan pada area kulit yang terkena
- CLM dapat terjadi di bagian tubuh mana saja, namun paling sering pada area yang kemungkinan sering terpapar tanah atau pasir yang terkontaminasi parasit, seperti kaki, bokong, paha, dan tangan
Karena lesi CLM bisa sangat gatal, orang dengan CLM cenderung menggaruk bagian tubuh yang terkena. Hal ini dapat merusak kulit dan meningkatkan risiko infeksi bakteri sekunder atau tambahan.
Diagnosis
Dokter dapat mendiagnosis CLM berdasarkan keluhan, riwayat aktivitas atau pekerjaan, serta melalui pemeriksaan lesi kulit yang khas. Jika Anda tinggal di daerah lembap atau tropis, informasi detail tentang lingkungan Anda sehari-hari dapat membantu dokter dalam menegakkan diagnosis.
Tata Laksana
CLM adalah penyakit yang bisa sembuh sendiri. Larva di bawah kulit biasanya mati dalam waktu 5 sampai 6 minggu tanpa pengobatan. Namun, pada beberapa kasus mungkin diperlukan waktu lebih lama untuk sembuh.
Penggunaan obat krim atau salep maupun obat minum dapat membantu infeksi sembuh lebih cepat. Dokter akan meresepkan obat antiparasit untuk membunuh cacing yang menginfeksi. Obat antiparasit yang beredar di Indonesia umumnya berupa obat minum. Selain meminum obat, dokter juga akan menyarankan untuk menjaga kebersihan kulit dengan mandi dua kali sehari menggunakan sabun.
Komplikasi
Komplikasi yang dapat terjadi akibat CLM antara lain:
- Rasa gatal yang bisa mengganggu aktivitas
- Infeksi bakteri sekunder, biasanya disebabkan oleh bakteri Staphylococcus aureus dan Streptococcus pyogenes, dapat menyebabkan selulitis atau infeksi meluas pada kulit dan jaringan di bawah kulit. Pada infeksi bakteri yang berkepanjangan, pernah dilaporkan adanya komplikasi radang ginjal pasca infeksi streptokokus
- Reaksi alergi akibat cacing
- Pada kasus yang langka, dilaporkan adanya sindrom Loeffler (sel darah putih eosinofil terkumpul di paru sebagai respon terhadap infeksi parasit)
Pencegahan
Jika Anda bepergian ke daerah endemik CLM, ada beberapa langkah yang dapat dilakukan untuk membantu mencegah infeksi:
- Kenakan sepatu atau alas kaki untuk mengurangi risiko terpapar tanah atau pasir yang terkontaminasi larva cacing
- Kenakan pakaian yang menutup paha dan bokong, area tubuh lainnya yang umum terkena infeksi CLM adalah paha dan bokong, yang dapat terpapar parasit saat sedang duduk atau berbaring
- Hindari duduk atau berbaring pada tempat yang berpotensi terkontaminasi karena dapat meningkatkan risiko kulit terpapar larva
- Gunakan handuk atau kain saat duduk atau berbaring di area yang mungkin terkontaminasi
- Jika memungkinkan, hindari area yang sering dikunjungi banyak hewan, terutama anjing dan kucing. Jika Anda harus melakukan perjalanan melalui area tersebut, gunakanlah alas kaki
- Pertimbangkan waktu dan musim saat akan bepergian, terutama perjalanan luar negeri. Beberapa daerah mengalami lonjakan infeksi CLM saat musim hujan
- Beberapa negara berkembang menerapkan pengobatan pencegahan kepada orang-orang yang berisiko tinggi terkena infeksi, seperti:
- Wanita hamil
- Anak-anak
- Memiliki pekerjaan yang banyak terpapar pasir, tanah, atau lebih berisiko terkena cacing tambang
Kapan Harus ke Dokter?
Jika Anda atau anak mengalami ruam kulit yang berbentuk khas dan disertai dengan keluhan infeksi CLM seperti yang disebutkan di atas, konsultasi dengan dokter sebelum infeksi meluas dan mengganggu aktivitas.
Mau tahu informasi seputar penyakit kulit dan rambut lainnya? Yuk, baca lebih banyak artikelnya di sini!
- dr Hanifa Rahma
Schulman, JS. (2019). About cutaneous larva migrans. Retrieved 14 March 2022, from https://www.healthline.com/health/cutaneous-larva-migrans
Robles, DT. (2020). Cutaneous larva migrans. Retrieved 14 March 2022, from https://emedicine.medscape.com/article/1108784-overview
Maxfield, L., Crane, JS. (2021). Cutaneous Larva Migrans. Retrieved 14 March 2022, from https://www.ncbi.nlm.nih.gov/books/NBK507706/
Cristol, H. (2020). Hookworms. Retrieved 14 March 2022, from https://www.webmd.com/a-to-z-guides/hookworm-infection
Montgomery, S. (2019). Cutaneous larva migrans. Retrieved 14 March 2022, from https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/cutaneous-larva-migrans
Reichert, F., Pilger, D., Schuster, A., Lesshafft, H., Guedes de Oliveira, S., Ignatius, R., et al. (2018) Epidemiology and morbidity of hookworm-related cutaneous larva migrans (HrCLM): Results of a cohort study over a period of six months in a resource-poor community in Manaus, Brazil. PLoS Negl Trop Dis 12(7): e0006662. https://doi.org/ 10.1371/journal.pntd.0006662