Definition
Filariasis is a chronic disease caused by parasitic infections that could last for a long time. Filariasis is synonymous with lymphatic filariasis or elephantiasis.
It is the second most prevalent disease that could result in enduring permanent disability globally. Filariasis can impact individuals of all age groups. The disease has a higher prevalence in men compared to women, with a ratio of 10:1.
Children can be infected by parasites that cause filariasis, but symptoms like leg swelling may only manifest later in life. If left untreated, filariasis can result in many problems, including temporary or permanent disabilities.
Causes
In tropical regions such as Indonesia, mosquitoes act as vectors for parasitic pathogens, transmitting the parasites to people. These parasitic organisms are roundworms known as Wuchereria bancrofti, Brugia malayi, and Brugia timori. Various kinds of mosquitoes, such as Aedes, Anopheles, Culex, Mansonia, and Ochlerotatus, carry these parasites. These mosquitoes will bite humans and transmit pathogens, leading to the spread of diseases. Mosquitoes can transmit many diseases, including filariasis.
Mosquitoes carry parasites that enter the human body through their saliva. Within the body, these pathogens spread via the lymphatic vessels and induce harm. Additionally, damage to the lymph vessels will result in obstruction and swelling of the hands, feet, breasts, and genitals.
The parasites proliferate in the human lymphatic vessels. Subsequently, immature larvae are released into the circulation. When a mosquito bites a human, it ingests blood that contains larvae. The immature larvae mature inside the mosquito's body. If a mosquito bites another human, it can transmit a filariasis infection through its saliva, carrying parasitic germs.
Risk factor
Various factors can increase the risk of filariasis, including:
- Residing near swamps
- Low income
- Possessing limited information, particularly regarding filariasis and ways to prevent it
- When sleeping, do not use mosquito nets or insect repellent.
- Wearing garments with exposed arm or leg areas makes it easier for mosquitoes to bite you.
Symptoms
Filariasis infection can manifest as asymptomatic, acute (recent onset or short-lived symptoms), or chronic. Most filariasis cases are asymptomatic, displaying no visible symptoms in the body. In these instances, even though they do not experience any symptoms, the individual is already infected, and the parasites can harm the lymphovascular system and kidneys and weaken the immune system.
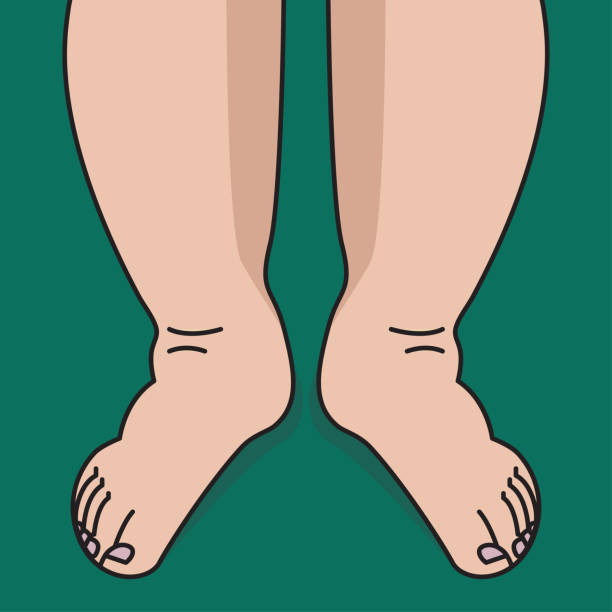
If the filariasis infection progresses to a chronic state, it will result in tissue swelling and skin thickening around the legs. Testicular swelling, known as hydrocele, is a frequent occurrence. Genital and breast swelling may also develop.
Diagnosis
Medical Interview
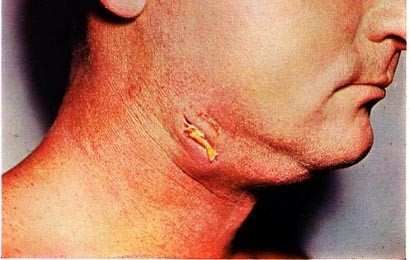
Your doctor will inquire about the symptoms you are experiencing, including fever, headache, fatigue, and chills. If you have filariasis with red, warm skin bumps, you may later experience swelling and pain in the affected area. The bumps may rupture, leading to the removal of dead adult parasites. Filariasis can lead to milky-white urine when lymph veins rupture and the discharges spill into the urinary system. Urine may appear scarlet due to the presence of blood, accompanied by pain in the groin and testicles and tiny swelling in the armpits and groin (lymphadenopathy).
Physical Examination
During the physical examination, your doctor will often assess the location of the swellings on the body, whether the swellings are present on the genitals, upper limbs, or lower limbs. When touched, the enlarged skin will feel firm and dense.
Diagnostic Tests
1. Laboratorium tests
Blood samples were collected after 8 p.m. This is done because the parasites are most active throughout the night. The blood samples will be examined in the laboratory using a microscope. If a person has filariasis, their blood test results will show elevated levels of white blood cells, particularly eosinophils.
2. PCR
This test is conducted to identify antigens produced by the pathogens. It is the favored diagnostic approach because it can identify occult or asymptomatic filariasis infections.
3. Scrotal ultrasound
This test is conducted on male patients suspected of having asymptomatic filariasis. During a scrotal ultrasound, the doctor will examine the movement patterns of the parasites responsible for filariasis, typically seen in the lymphatic systems.
Management
Medications
To treat filariasis, your doctor will prescribe antiparasitics to target the parasites responsible for the disease. The doctor might also prescribe antibiotics (doxycycline) to the patient, particularly if they reside in a region where Loa loa, a type of roundworm that can lead to filariasis, is prevalent.
Surgical Procedures
Aside from antiparasitic drugs, surgery is another treatment option for filariasis. Surgeons perform this procedure to repair the lymphatic drainage channels compromised by the parasites responsible for filariasis.
Chronic filariasis can lead to recurrent edema of lymphatic vessels. To address this issue, your doctor will recommend maintaining skin hygiene, wearing comfortable shoes, routinely washing your body with soap and clean water, elevating your limbs, and utilizing compression bandages.
Complications
Untreated filariasis can result in various complications. Lymphatic filariasis causes skin thickening and calf swelling. Moreover, this might result in both temporary and permanent disabilities.
Filariasis-induced disability might result in social stigma and mental health problems for the affected individuals. It can also reduce income opportunities and higher medical expenses for patients and caregivers. Filariasis leads to a significant social and economic impact.
Furthermore, filariasis can lead to tropical pulmonary eosinophilia syndrome. This illness arises from elevated eosinophils caused by filariasis infection in the lungs, leading to coughing and shortness of breath.
Prevention
Filariasis is transmitted via the secretions of mosquitoes' saliva infected with the parasitic microorganisms responsible for the disease. To avoid filariasis, you can take many measures, such as:
- Sleeping in an air-conditioned room or beneath a mosquito net at night is advisable.
- Wear long clothing, such as long sleeves and slacks, and apply mosquito-repellent cream to your skin.
- In cases of filariasis infection, health centers typically offer mass distribution of anti-filariasis medication to eradicate the parasitic organisms responsible for filariasis, regulate mosquito population growth, and reduce disease transmission.
When to see a doctor?
If you observe any signs of abnormal swelling, pain, and inflammation in your feet, consult a doctor immediately.
Looking for more information about other diseases, Check here!
- dr Hanifa Rahma
Newman, TE, Juergens AL. Filariasis. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556012/
Zulfiqar H, Malik A. Bancroftian Filariasis. [Updated 2022 Jan 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547682/
Maryen, Y., Kusnanto, H., & Indriani, C. (2018). Risk Factors of Lymphatic Filariasis in Manokwari, West Papua. Tropical Medicine Journal, 4(1), 62.
CDC.gov. (2020, 26 Oktober). Parasites-Lymphatic Filariasis Prevention & Control. Diakses pada 16 Maret 2022, dari https://www.cdc.gov/parasites/lymphaticfilariasis/prevent.html
WHO.int. Lymphatic filariasis (Elephantiasis) Treatment. Diakses pada 16 Maret 2022, dari https://www.who.int/health-topics/lymphatic-filariasis#tab=tab_3
Clevelandclinic.org. (2021, 15 Oktober). Filariasis. Diakses pada 16 Maret 2022, dari https://my.clevelandclinic.org/health/diseases/21925-filariasis
WHO.int. (2022, 16 Maret). Lymphatic Filariasis. Diakses pada 16 Maret 2022, dari https://www.who.int/news-room/fact-sheets/detail/lymphatic-filariasis