Definisi
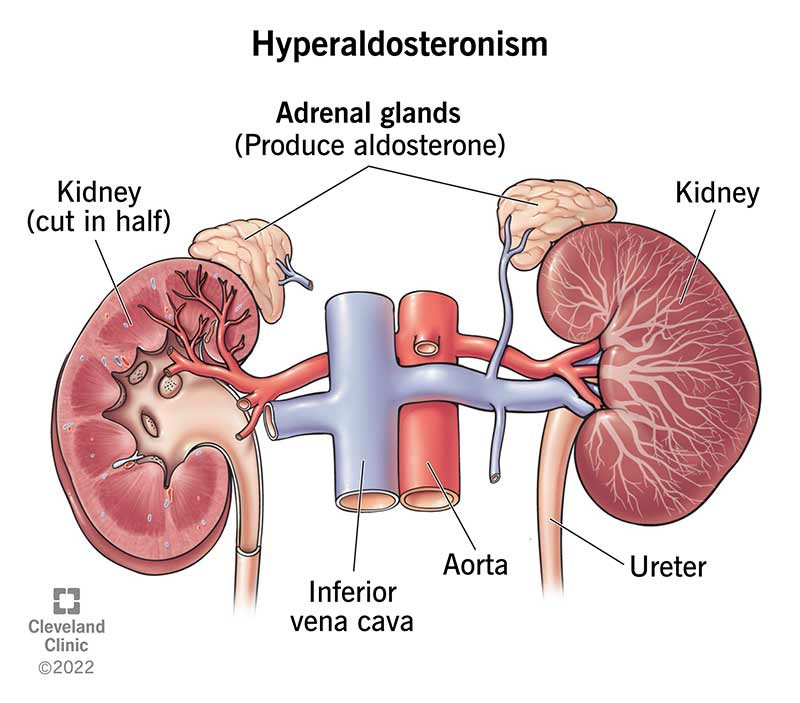
Hiperaldosteronisme adalah suatu kelainan dimana salah satu atau kedua kelenjar adrenal memproduksi terlalu banyak hormon aldosteron ke dalam darah. Hormon aldosteron adalah hormon yang membantu meregulasi tekanan darah dengan cara mengontrol kadar kalium dan natrium dalam darah.
Kelenjar adrenal merupakan bagian dari sistem endokrin. Sistem endokrin memproduksi hormon yang dibutuhkan tubuh untuk melakukan fungsinya sehari-hari. Tubuh memiliki dua kelenjar adrenal, yaitu satu di atas setiap ginjal.
Hiperaldosteronisme dikelompokkan menjadi dua, yaitu:
- Hiperaldosteronisme primer (sindrom Conn): terdapat gangguan dalam kelenjar adrenal yang menyebabkan terlalu banyak hormon aldosteron dilepas
- Hiperaldosteronisme sekunder: terdapat gangguan pada bagian tubuh yang lain sehingga kelenjar adrenal memproduksi terlalu banyak hormon aldosteron
Hiperaldosteronisme dapat menyebabkan tekanan darah tinggi (hipertensi) dan kadar kalium darah yang rendah.
Jika Anda ingin mengetahui selengkapnya mengenai hipertensi, Anda dapat membacanya di sini: Hipertensi - Definisi, Penyebab, Gejala, dan Pengobatannya
Penyebab
Hiperaldosteronisme memiliki beberapa penyebab yang berbeda bergantung pada tipenya primer atau sekunder.
Hiperaldosteronisme primer terjadi ketika terdapat gangguan pada kelenjar adrenal yang menyebabkannya memproduksi terlalu banyak hormon aldosteron. Adenoma adrenal (tumor non kanker) adalah penyebab hiperaldosteronisme primer yang paling banyak.
Penyebab hiperaldosteronisme primer yang lebih jarang meliputi:
- Hiperplasia adrenal unilateral (pembesaran salah satu kelenjar adrenal)
- Karsinoma adrenokortikal yang memproduksi aldosteron (tumor ganas)
- Hiperaldosteron familial tipe 1 (sutu kondisi yang diturunkan dari orang tua kandung)
Hiperaldosteronisme sekunder disebabkan oleh menurunnnya aliran darah ke ginjal. Untuk memahami bagaimana hal ini terjadi, penting untuk mengetahui bahwa aldosteron adalah bagian dari rekasi hormonal kompleks yang meregulasi tekanan darah. Hal ini disebut dengan sistem renin-angiotensin-aldosteron, dan sistem ini melibatkan langkah dibawah ini:
- Ginjal melepaskan enzim renin ketika tubuh mendeteksi tekanan darah rendah atau kadar natrium darah yang rendah. Renin mengubah angiotensinogen (suatu precursor angiotensin yang diproduksi oleh hati) menjadi angiotensin I (angiotensin adalah hormon yang mempersempit pembuluh darah).
- Angiotensin I diubah menjadi angiotensin II
- Angiotensin II mempersempit pembuluh darah dan menstimulasi pelepasan aldosteron
Penurunan aliran darah ke ginjal akan mencetuskan sistem renin-angiotensin-aldosteron, yang mengakibatkan kelebihan aldosteron di tubuh Anda.
Penyebab menurunnya aliran darah dan hiperaldosteronisme sekunder, meliputi:
- Penyakit arteri renal obstruktif
- Hipertensi renal
- Kondisi yang menyebabkan penumpukan cairan dalam tubuh, seperti gagal jantung, sirosis hati, dan sindrom nefrotik
Baca Juga: Sindrom Nefrotik - Definisi, Penyebab, Gejala, dan Pengobatannya
Faktor Risiko
Kondisi ini paling sering terjadi apda orang berusia 30-50 tahun dan merupakan penyebab yang sering dari tekanan darah tinggi pada orang berusia paruh baya. Kondisi ini juga lebih sering terjadi pada perempuan dibandingkan dengan laki-laki.
Sulit untuk para ahli memperkirakan seberapa sering hiperaldosteronisme terjadi. Beberapa studi mengatakan bahwa sekitar 5-10% penderita tekanan darah tinggi menderita hiperaldosetronisme primer. Para ahli memperkirakan sebanyak 25% orang dengan tekanan darah tinggi yang resisten obat dapat menderita hiperaldosteronisme.
Gejala
Gejala hiperaldosteronisme dapat bervariasi bergantung pada tingkat keparahan kondisi tersebut. Beberapa orang dengan hiperaldosteronisme yang ringan tidak memiliki gejala (asimtomatik).
Gejala hiperaldosteronisme yang paling banyak yaitu tekanan darah tinggi (hipertensi), terutama hipertensi yang resisten terhadap obat.
Jika Anda mengalami gejala lainnya, gejala tersebut kemungkinan disebabkan oleh tekanan darah tinggi sedang sampai berat dan/atau kadar kalium yang rendah (hipokalemia).
Gejala tekanan darah tinggi meliputi:
- Nyeri kepala
- Pusing
- Gangguan penglihatan
- Sesak nafas
Gejala kalium rendah meliputi:
- Kelemahan otot (pada kasus yang berat dapat menyebabkan kelumpuhan sementara)
- Ketegangan otot
- Kesemutan dan mati rasa
- Kelelahan
- Rasa haus yang berlebihan (polidipsia)
- Sering berkemih
Diagnosis
Dokter akan mendiagnosis hiperaldosteronisme dengan pemeriksaan darah. Namun, banyak orang dengan hiperaldosteronisme tidak terdiagnosis karena banyak kondisi dan faktor risiko yang juga dapat menyebabkan tekanan darah tinggi.
Tanda umum hiperaldosteronisme yaitu tekanan darah tinggi yang resisten terhadap obat dan disertai dengan hasil pemeriksaan darah panel elektrolit yang abnormal, seperti:
- Kenaikan kadar natrium ringan (hipernatremia)
- Penurunan kadar magnesium ringan (hipomagnesia)
Jika dokter mencurigai bahwa Anda kemungkinan mengalami hiperaldosteronisme berdasarkan tanda dan gejala, dokter akan melakukan pemeriksaan darah yang disebut konsentrasi renin plasma atau aktivitas renin plasma.
Jika Anda mengalami hiperaldosteronisme primer, hasil kedua pemeriksaan tersebut akan lebih rendah dari normal. Sebaliknya, pada hiperaldosteronisme sekunder hasilnya akan lebih tinggi dari normal.
Anda juga kemungkinan membutuhkan tes supresi aldosteron. Tes ini dilakukan dengan mengkonsumsi sejumlah natrium (garam) melalui mulut atau cairan infus selama waktu tertentu. Anda akan memberikan sampel urine selama 24 jam sehingga laboratorium dapat mengukur kadar aldosteron dalam urine Anda.
Jika pemeriksaan ini mengkonfirmasi Anda mengalami hiperaldosteronisme dokter akan merekomendasikan pemeriksaan tambahan untuk menentukan penyebabnya. Sebagai contoh, dokter dapat merekomendasikan pemeriksaan radiologi seperti CT scan untuk mencari adanya tumor yang dapat menyebabkan hiperaldosteronisme.
Prosedur diagnosis lainnya dapat dilakukan dengan memasukan kateter atau selang ke dalam pembuluh darah kelenjar adrenal. Hal ini dilakukan untuk membantu memeriksa kelenjar adrenal yang mana (dari dua kelenjar adrenal) yang memproduksi terlalu banyak hormon aldosteron. Pemeriksaan ini penting karena banyak orang yang memiliki tumor jinak berukuran kecil di kelenjar adrenal yang tidak memproduksi hormon sedikitpun. Berpatokan pada hasil CT scan saja dapat menyebabkan pengangkatan kelenjar adrenal yang salah.
Tata Laksana
Hiperaldosteronisme primer yang disebabkan oleh tumor kelenjar adrenal sering ditangani dengan operasi. Namun, terkadang kondisi ini dapat ditangani dengan pemberian obat-obatan.
Pengangkatan tumor kelenjar adrenal dapat mengontrol gejala. Bahkan setelah operasi, beberapa orang tetap mengalami tekanan darah tinggi dan perlu mengkonsumsi obat-obatan. Namun, seringnya jumlah dan dosis obat dapat diturunkan setelah operasi.
Pembatasan konsumsi garam dan konsumsi obat teratur dapat mengontrol gejala tanpa operasi. Obat untuk menangani hiperaldosteronisme, meliputi:
- Obat yang menghambat aksi aldosetron
- Diuretik, untuk membantu mengontrol penumpukan cairan di dalam tubuh dengan membuangnya lewat urine
Hiperaldosetronisme sekunder ditangani dengan obat-obatan di atas dan pembatasan asupan garam. Operasi biasanya tidak dilakukan.
Komplikasi
Hiperaldosteronisme primer dapat menyebabkan tekanan darah yang sangat tinggi, yang dapat merusak banyak organ, termasuk mata, ginjal, jantung, dan otak. komplikasi paling sering adalah gangguan pada jantung dan pembuluh darah, yang meliputi:
- Atrium Fibrilasi (gangguan irama jantung)
- Hipertrofi ventrikel kiri (penebalan otot jantung)
- Serangan jantung
- Strok
Gangguan ereksi dan ginekomastia (pembesaran jaringan payudara pada pria) dapat terjadi akibat konsumsi obat-obatan penghambat efek hiperaldosteronisme jangka panjang.
Baca Juga: Ginekomastia - Definisi, Penyebab, Gejala, dan Pengobatannya
Pencegahan
Pada kebanyakan kasus, tidak ada yang dapat Anda lakukan untuk mencegah hiperaldosteronisme.
Kapan Harus ke Dokter?
Jika Anda sudah terdiagnosis hiperaldosteronisme, Anda perlu untuk mengunjungi dokter secara teratur untuk memastikan dosis pengobatan Anda sudah tepat.
Anda sebaiknya menghubungi dokter jika Anda menyadari adanya gejala baru atau jika gejala Anda mengalami perubahan.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr. Monica Salim
Hyperaldosteronism (2021) Pennmedicine.org. Available at: https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/hyperaldosteronism (Accessed: April 14, 2023).
Hyperaldosteronism: What it is, causes, symptoms & treatment (2022) Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/diseases/16448-hyperaldosteronism (Accessed: April 14, 2023).
Grossman, A.B. (2022) Hyperaldosteronism - hormonal and metabolic disorders, MSD Manual Consumer Version. MSD Manuals. Available at: https://www.msdmanuals.com/home/hormonal-and-metabolic-disorders/adrenal-gland-disorders/hyperaldosteronism (Accessed: April 14, 2023).